The smart investment in global health
This is a guest blog by Lenio Capsaskis, Health Advocacy Adviser, Save the Children UK. The blog originally appeared on Save the Children UK.
“Universal health coverage is a smart investment. Not just for health, but for all the Global Goals. It reduces poverty and drives prosperity.” Alok Sharma, former Secretary of State for International Development, Speech at the UN-High Level meeting on UHC.
This month marks one year since the first ever UN High-Level Meeting on Universal Health Coverage. World leaders came together and unanimously adopted a resolution agreeing to allocate resources towards achieving “financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all”.
When it comes to global public health the Foreign, Commonwealth and Development Office (FCDO) has big shoes to fill. The UK is the second largest government donor in global health, leading the way in areas such as anti-microbial resistance, advocating for women’s sexual and reproductive health and rights, and coming together with critical partners to support and promote childhood immunisation. But a new Stocktake Review produced by Action for Global Health shows there is a lot of work to be done if the UK wants to lead on global efforts to achieve universal health coverage (UHC).
IS UHC LOSING STEAM?
With the new department’s priorities starting to form, and the fiscal situation becoming clearer, global health advocates are worried that health systems and UHC are falling down the agenda. In a July letter, Foreign Secretary Dominic Raab outlined the new department’s priorities: “tackling climate change and reversing biodiversity loss, championing girls’ education, UK leadership in the global response to COVID-19, and campaigning on issues such as media freedom and freedom of religious belief”.
While heartened by the reference to COVID-19, there is growing concern that financial protection for the most deprived and marginalised communities, which doesn’t make for easy ‘soundbites’ or fit squarely in the national interest, will disappear altogether. Recent Save the Children analysis in this blog series confirms there has been a redistribution of UK aid to COVID-19 related areas of the health budget, at the expense of other critical interventions for ending preventable deaths and improving overall health and wellbeing. Even more cuts are expected in the 2021– 22 budgeting period.
Health security, recovery from COVID-19 and UHC are inextricably linked; continuing to invest in all three is the smart thing to do. Strong and resilient health systems are critical in responding to COVID-19 – including the need to continue to deliver essential services. Public investment in health systems is the most equitable way to finance UHC and ensure financial protection for the most vulnerable people. COVID-19 will only increase pressure on national health systems around the world and paying for care will inevitably push people into further poverty. Our new policy brief, Build Back Better to Deliver Health for All, provides evidence that countries with lower levels of public investment in health have faced larger disruptions to essential services. This is the time for the FCDO to ramp up its support to domestic revenue mobilisation and allocation to resilient public health systems.
IN THE GLOBAL INTEREST: PROTECTING PUBLIC FINANCING FOR HEALTH
To deliver on its global health objectives, the FCDO might look to the private sector to forge greater links with international trade and business. Blended finance for health, linked to the private sector, was US$1.8 billion in 2017 (0.1% of total health finance) – an increase by a factor of almost 20 since 2012. Undoubtedly, the private sector is recognised as a critical partner for achieving UHC, but it will be very important that the UK remains committed to closing the equity gap in low- and middle-income countries. In many resource-poor settings healthcare is not free at the point of use and as a result, every year around 100 million people are pushed into extreme poverty paying for healthcare. Reports have shown that voluntary private and community-based health insurance schemes are ineffective for achieving UHC and lead to the exclusion of the most marginalised members of society.
Further, we know that the UK government is exploring innovative ways to make markets work for development. The CDC Group is seeking to scale up its investments in health care as a response to the COVID-19 pandemic. There are concerns, in an evaluation conducted for the CDC Group, that patients at one of its own investments, the Narayana Health hospital chain in India, are not protected against catastrophic health expenditure.i Scaling up this model of health service provision may sound attractive to investors, and therefore align with the FCDO’s trade and diplomatic goals, but the reality is that the risk of using government funds to perpetuate inequities is far too high.
WHERE IS THE FCDO NEEDED MOST?
The COVID-19 pandemic shows us that markets have not worked to bring forward investments in much needed ‘common goods for health’ as outlined by the World Health Organization. Investing in public health systems as an insurance policy to avoid the havoc that pandemics wreak and to ensure long-term good health rather than treatment of ill health does not sell. That’s why national governments in low- and middle-income countries, with support from donors like the FCDO, must prioritise public financing.
Alongside its direct support for public health systems, the FCDO should also support governments to increase their fiscal space, to enable further investment in health, such as though supporting domestic revenue mobilisation (DRM) or through debt relief. While the UK government has recently supported the IMF Catastrophe Containment and Relief Trust, enabling 26 of the world’s poorest countries to receive short-term debt relief, its commitment to double support to domestic revenue mobilisation under the Addis Tax Initiative (ATI) is set to be missed (Figure 1).
Figure 1. FCDO budget for this financial year shows the ATI target is set to be missed
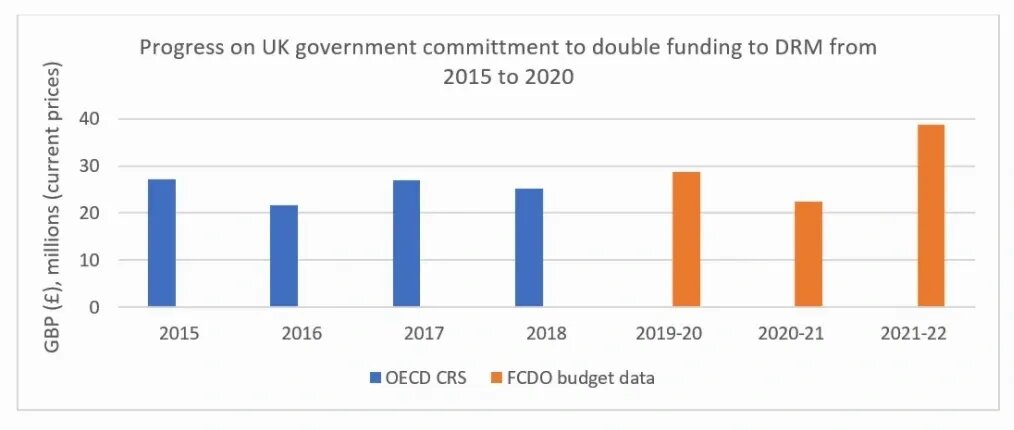
Source: OECD Credit Reporting System, iati.fcdo.gov.uk accessed through the IATI registry (August 2020 update)
In addition, research has shown only 7% of donors’ support to DRM contained clear goals related to equity or fairness. To promote prosperity and equity globally, the UK must lead the way in supporting increased tax capacity and progressive taxation for health, which is an under-resourced and much needed pillar of any public health response and plan. Only then will we able to achieve global health security as a fundamental part of universal health coverage.
Read more from Save the Children’s blog series on The Future of British Aid.